Discospondylitis in Pets: Signs, Diagnosis & Treatment
November 15, 2016Discospondylitis is an infection (-itis) of the intervertebral disc (disco-) and adjacent vertebral endplates (spondylo-). It is most often due to a bacterial infection, but fungal organisms are occasionally identified. The most commonly isolated organisms are Staphylococcus aureus, S. intermedius, Brucella canis, andEscherichia coli. Other microbes that have been reported include Streptococcus, Staphylococcus pseudintermedius, Klebsiella, Pseudomonas, Proteus, Candida tropicalis, and Actinomyces pyogenes. The most commonly reported fungal organism is Aspergillus.
Colonization of the intervertebral discs can occur through hematogenous spread (often secondary to a urinary tract infection), direct inoculation (e.g., trauma, foreign body migration), or iatrogenic infection (e.g., neurosurgery, intramuscular injections).
Signalment
Discospondylitis is most common in large and giant breed dogs, but can occur in any breed of dog. It also occasionally occurs in cats. In one large retrospective study of 513 dogs, Great Danes, Boxers, Rottweilers, English Bulldogs, German Shepherd Dogs, and Doberman Pinschers were at higher risk of disease. This disease occurs at all ages, but is most common in middle-aged to older dogs. Male dogs are more commonly affected.
Clinical signs
Patients with discospondylitis frequently are presented with chronic, progressive signs of vertebral hyperesthesia and a stiff, stilted gait. Acute onset of clinical signs is possible. Clients frequently report non-specific signs of decreased appetite, lethargy, weight loss, and reluctance to move. In some cases, clinical signs progress to inability to walk.
Neurologic & physical exam
As with the majority of neurological disorders, clinical signs reflect lesion location and are not specific to any particular disease. In the same large retrospective study described above, 52% of the dogs had a normal neurological exam other than hyperesthesia on palpation of the vertebral column. The remaining 48% of patients showed varying degrees of neurological dysfunction, including paraparesis (27 dogs), postural reaction deficits only (14), paraplegia with absent deep pain perception (7), paraplegia with intact pain sensation (6), and tetraparesis (5).
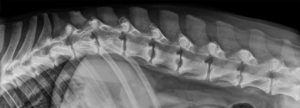
Lateral radiograph of a dog with discospondylitis at L1-2, L2-3, and L4-5. Image courtesy of Dr. Allison Zwingenberger, www.veterinaryradiology.net
Diagnosis
Discospondylitis is usually diagnosed radiographically. The classic radiographic signs of discospondylitis are collapsed intervertebral disc space with lysis of the adjacent vertebral end plates and variable endplate sclerosis. Multiple discs are affected in 40% of patients so radiographs of the entire vertebral column should be obtained (fig 1.).
The minimum database for discospondylitis is a complete blood count (CBC) and biochemical profile. Leukocytosis is occasionally seen on CBC, but the remainder of routine blood tests are usually normal. Urinalysis with urine culture & sensitivity and blood cultures are recommended. Only 40% of patients will have a positive urine and/or blood culture. However, positive culture results are highly correlated to the organism causing the discospondylitis. Brucella titers should be performed on all patients because it is a zoonotic disease. Although more common in sexually intact dogs, Brucella discospondylitis can occur in sexually altered dogs. Thoracic radiographs and abdominal ultrasound are recommended to evaluate for other concurrent diseases.
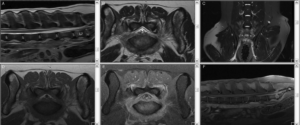
MRI of a dog with L7-S1 discospondylitis and secondary neuritis and myositis. Top row is sagittal (A), transverse (B) and dorsal (C) T2-weighted images. The bottom row is pre- (D) and post-contrast T1-weighted transverse (E) and sagittal (F) images.
Radiographic changes of discospondylitis may not be visible until 2-4 weeks after onset of clinical signs. As result, diagnosis via advanced imaging is increasingly common, especially when performed early in the course of illness. MRI is the imaging modality of choice (fig. 2), but changes may also be apparent on CT. The classic MRI appearance of discospondylitis is collapse of the intervertebral disc space with a hyperintense signal on T2-weighted and STIR in the affected disc and hypointensity of the vertebral endplates on T1-weighted images. Moderate to marked contrast enhancement of the disc, endplates, and paravertebral tissues is usually present.
Treatment
Antibiotic choice is ideally based on isolation of the organism via disc aspiration or surgical curettage. Since discospondylitis is caused most often by Staphylococcus, Streptococcus, or E. coli, empirical treatment is acceptable in many cases. The antibiotic chosen should have good bone penetration. Most patients will respond to a cephalosporin (e.g., cephalexin) or potentiated penicillin (e.g., Clavamox). Cephalexin is used most often because it is inexpensive and usually effective. Treatment should be continued long term. Many sources frequently recommend treating for 2-3 months minimum or a certain amount of time (e.g., 2 weeks) beyond clinical and/or radiographic resolution. However, radiographic resolution is slow and may not occur. In this author’s experience, many patients need to be treated long term (6-12 months or longer) as signs may recur if antibiotics are stopped too soon. If there is a poor response to the initial antibiotic, intervertebral disc culture & sensitivity is recommended if not already performed.
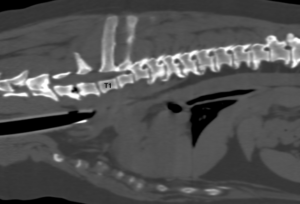
2D orthogonal MPR image of a dog undergoing CT imaging to further investigate a possible heart or lung mass. Discospondylitis was noted at C6-7 and T4-5 (not readily apparent in this image), which was later confirmed on MRI that was performed to investigate the patient’s primary clinical sign of pain when opening the mouth.
Fungal infection should always be considered in dogs that are not responding quickly to antibiotics. German Shepherd Dogs appear to be predisposed to Aspergillus infection. Anti-fungal medications should be started if a fungal organism is isolated.
Treatment of brucellosis is difficult and combination therapy is required.
- The treatment of choice is minocycline 10 mg/kg PO q12h for 4 weeks and streptomycin (20 mg/kg IM or SQ q24h during weeks 1 and 4 of treatment).
- Streptomycin is unavailable in the USA so it can be replaced with gentamicin (5 mg/kg IM or SQ q24 during weeks 1 and 4 of treatment).
- A safer combination used by many is doxycycline (5 mg/kg PO q12h) and enrofloxacin (5 mg/kg PO q24h).
Brucellosis is an incurable disease, but patients may have a good quality of life with long-term (possibly life-long) antibiotics. Owners of brucellosis patients should be informed of its zoonotic potential and the need for good hygiene. Brucellosis is a reportable disease in most areas. Neutering or spaying the dog is recommended.
Pain medications should be instituted early in the course of disease. Patients with mild to moderate pain may respond to:
- Non-steroidal anti-inflammatory drugs
- Gabapentin
- Tramadol or transdermal Fentanyl (for acute, short-term pain relief)
- Acetaminophen with codeine may be helpful in refractory cases
For moderate to severe pain, stronger medications, such as injectable or continuous rate infusion of pure opioid (e.g., fentanyl, hydromorphone) +/- other medications (e.g., dexmedetomidine, ketamine, lidocaine) should be considered.
Occasionally, surgery needs to be performed to decompress the spinal cord and/or stabilize the spine.
Prognosis
The prognosis is generally good to excellent for bacterial discospondylitis if the disease is treated early and aggressively. Fungal discospondylitis has a fair to guarded prognosis and may require long-term treatment. Brucellosis cannot be cured, but patients can have an acceptable quality of life with long-term treatment.